The Well for Health Promotion promotes sexual health by providing programs, services, and resources that are inclusive, holistic, and evidence-based. Our staff at The Health Center provides high quality, medical sexual health care.
Sexual Health Services
Student Health Center Services
Sexual and reproductive health is an important part of your overall well-being. The clinicians at the Health Center offer many services to Tulane students that support most common sexual and reproductive health needs. These services include STI testing, pre-exposure prophylaxis, gynecological services and screenings, transgender health services, and many others. For more information, please visit the link below or call 504-865-5255 (Uptown) or 504-988-6929 (Downtown) during business hours.
At Tulane, Campus Health offers two types of STI testing options:
GYT Clinic
A quick and easy way for Tulane students to get screened for sexually transmitted infections (STIs).
- Screenings are for those who have no symptoms and no recent exposure to an STI.
- Test screen for HIV, Gonorrhea, and Chlamydia.
- There are no limits on how many times a student can use GYT.
- GYT visits are confidential and are not recorded for insurance claims.
To make a GYT appointment, please call the Student Health Center Uptown at 504-865-5255 or the Student Health Center Downtown at 504-988-6929.
Learn more about GYT screening
STI Testing
A comprehensive appointment that includes STI testing and doctor’s consultation.
- STI testing is provided as a medical appointment that is submitted to your health insurance.
- Testing screen for HIV, Gonorrhea, and Chlamydia, Genital Herpes, Syphilis, Trichomoniasis, and HPV.
Check out this video with frequency asked questions about the STI/GYT Clinics:
Most of us "know" what menstruation is but we never actually learned all the facts about "getting your period." To learn about what menstruation is, why it happens, and how to relieve period pain, check out this video:
Free Menstrual Health Supplies
Tulane University offers free menstrual health supplies including tampons, pads, and liners in a variety of sizes to all Tulane students. You can access free menstrual products at the following locations:
- Uptown Campus - Safer Sex Supply Kiosk at the Student Health Center (building #92, 1st floor, in lobby by pharmacy)
- Downtown Campus - the all gender and gendered restrooms located in Tidewater, Elk Place, and Murphy.
Safer Sex Supplies
The Well for Health Promotion provides free safer sex supplies to all Tulane students.
The Well for Health Promotion provides free safer sex supplies to all Tulane students. Pick up supplies for yourself at the following Uptown locations:
- Safer Sex Supply Kiosk (1st floor, in lobby by Pharmacy) and all patient bathrooms at the Student Health Center (at corner of Willow & Newcomb, building #92)
- Locker rooms and all gender bathrooms in the Reily Center
- The Carolyn Barber Pierre Center for Intercultural Life in all gender bathroom (Richardson Building, 1st Floor)
- The Goldman Center for Student Accessibility (Howard-Tilton Library, Basement Floor)
- Student Organization Center (SOC) (LBC, Garden Level- Suite G11)
- Office of the Dean of Students/Student Resources & Support Services (LBC, Garden Level- Suite G02)
- Office of Fraternity and Sorority Programs- (LBC, Garden Level- Suite G04)
- The Q-Spot (located in Décou-Labat Residence Hall on the ground level right next to/behind PJ's on Willow)
- All residence halls
Pick up supplies for yourself at the following Downtown locations:
- Elk Place- 2nd and 3rd Floor restrooms
- Tidewater- 1st and 12th Floor restrooms
- Murphy- 5th Floor restrooms, 6th Floor Lounge restrooms
- Hutchinson- 1st Floor restrooms
If you are staff, faculty, an RA/RD, student organization, or FSL organization, you can request safer sex supplies to give out in your spaces, classes, and events.
Safer sex supply options
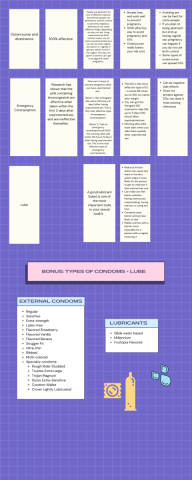
- External Condom Kit— 4 external condoms, 2 lubes, and a safer sex supply demonstration reference card.
- External condoms are Lifestyle brand and latex, unless labeled latex-free.
- External condom varieties include: Regular, Sensitive, Extra-Strength, Latex-free, Snugger fit, Ultra-thin, Ribbed, Multi-colored, Rough Rider Studded, Trustex Extra Large, Trojan Magnum, Durex Extra-Sensitive, Crown Lightly Lubricated
- Flavored External Condom Kit (for oral sex only)-- 2 flavored external condoms, 2 flavored lubes, and a safer sex supply demonstration reference card
- Flavored external condoms are Lifestyle brand and flavored strawberry, vanilla, banana, etc.. Lube is ID Fruitopia flavored strawberry, vanilla, etc.
- Dental Dam Kit (for oral sex only)-- 1 Dental dam, 1 unflavored lube, 1 flavored lube, and a safer sex supply demonstration reference card
- Dental Dams are flavored Latex and Line One Labs brand. Lubricant is ID Glide Water Based (unflavored) and ID Fruitopia (flavored).
For videos with step by step instructions for how to use dental dams, internal condoms, external condoms, and lube, click here.
Contraceptives or Birth Control
What is the difference between hormonal and non-hormonal birth control?
What types of hormonal birth control exist?
What types of non-hormonal birth control exist?
I am Trans. Do I need birth control?

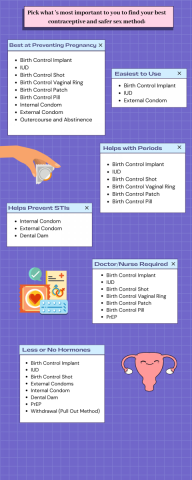
How to Choose Safer Sex Supplies or Contraceptives
There are many methods of contraception to choose from and it is worth taking the time to find out more about each one so that you can choose contraception that suits you. If you are still not sure talk to your healthcare provider about the best method for you.



Tulane and Loyola students may walk into the pharmacy at the Student Health Center and receive free emergency contraction during open business hours. Students are not required to have a health insurance plan nor do they need a prescription to access the emergency contraception.
What is EC?
Emergency contraception (aka the morning after pill) is birth control that you use after you have had unprotected sex—if you did not use birth control or your regular birth control failed. Emergency contraception should be used as soon as possible within three to five days after unprotected sex to prevent pregnancy. ECPs are more effective the sooner you take them. Emergency contraception does not work if you are already pregnant.
You can use emergency contraception to prevent pregnancy if:
- you didn’t use a condom or other birth control method when you had vaginal sex
- you messed up your regular birth control (forgot to take your birth control pills, change your patch or ring, or get your shot on time) and had vaginal sex
- your condom broke or slipped off after ejaculation (cumming)
- your partner didn't pull out in time
- you were forced to have unprotected vaginal sex
If you use emergency contraception correctly after you have unprotected sex, it makes it much less likely that you’ll get pregnant. But don’t use it regularly as your only protection from pregnancy, because it’s not as effective as regular, non-emergency birth control methods (like the IUD, pill, or condoms).
What types of emergency contraception exists?
There are 2 types of morning-after pills:
A pill with levonorgestrel. Brand names include: Plan B One Step, Take Action, My Way, AfterPill, and others.
- You can buy these morning-after pills over the counter without a prescription in most drugstores and pharmacies.
- Pan B is available for free without a prescription at the Student Health Center Pharmacy.
- These types of morning-after pills work best when you take them within 72 hours (3 days) after unprotected sex, but you can take them up to 5 days after. The sooner you take them, the better they work.
- These types of morning-after pills work best on people who weigh under 155 lbs.
A pill with ulipristal acetate. There’s only one brand, called ella.
- You need a prescription from a nurse or doctor to get ella emergency contraception.
- Make an appointment with the Student Health Center for an ella prescription that can be filled at the pharmacy.
- ella is the most effective type of morning-after pill.
- You can take ella up to 120 hours (5 days) after unprotected sex, and it works just as well on day 5 as it does on day 1.
- This type of morning-after pill work on people of all bodyweights.
Sex Education
The Well for Health Promotion provides a variety of peer and professional staff led workshops by request. These workshops include Sexual Health Jeopardy, the Consent Conversation, Medical Sex, Gender, and Sexual Orientation, Safer Sex Methods, Sexual & Reproductive Anatomy, and STI Prevention and Testing.
How to use Dental Dams
How to use External Condoms
How to use Internal Condoms
The Low Down on Lube
What is PrEP/PEP and Why Use It?
Why are they called STDs vs STIs?
While the terms can be used interchangeably, Sexually Transmitted Infection (STI) is often used instead of Sexually Transmitted Disease (STD). This is because STI is inclusive of both symptomatic and asymptomatic infections. Using the term STI also helps reduce stigma, especially since they are so common—more than half of all of us will get an STI at some point in our lives and 1 in 3 sexually active people under the age of 25 has an STI.
How can I protect myself from spreading or getting an STI?
Although anyone who is sexually active can get an STI, there are lots of ways to protect yourself and your partner(s):
- Use an internal or external condom or a dental dam, which are all available for free at the Well for Health Promotion!
- Get the HPV vaccine
- Consider medications like pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP) which prevents HIV infection Get tested.
- Getting testing is the most effective way for sexually active individuals to remain STI-free.
How do I know if I have an STI?
The only way to know you have an STI is to get tested. The most common STI symptom is actually a lack of symptoms or mild symptoms that get disregarded for something else. This means that most people with STIs don’t even know they have one until they get tested. Not getting treatment can also lead to long term health effects such as infertility, urinary tract and liver problems, and cancers. No STI is harmless so it’s best to get tested and treated!
How soon can I be tested?
Some STIs can be treated within a few days, while others take weeks or even monthly to become detectable. A window period is the time it takes for STIs to become detectable by If you have been exposed to an STI and are tested while in the window period, your test result may not be as accurate. The window period is 10 days for the chlamydia and gonorrhea test, and 3 months for the HIV test. It is best to schedule an appointment when you are out of the window period, if possible. It's important to note that you can still transmit STIs to your partner while you are in the window period.
How often should I get tested?
This depends. If you are sexually active, you should aim to be tested at least once per year. If you engage with multiple partners, it’s a good idea to get tested more frequently, perhaps every 3-6 months. If you’ve had unprotected sex, have a new partner (or more than one partner), or for any reason are worried you have been exposed to an STI, talk to your healthcare provider about getting tested. The bottom line is that it is up to you and it depends on you and your lifestyle!
When is STI testing appropriate?
If you're sexually active, it’s important to get tested on a regular basis, especially if you have more than one partner
- If you've had unprotected sex, have a new partner, or for any reason are worried you have been exposed to an STI
- If you have symptoms such as rash, sores, bumps, itching, burning, pain, odor, discharge, and/or bleeding in your genital region
- If you had a recent experience of sexual assault/sexual violence**
- If any of the above apply to you, talk to your healthcare provider about getting tested.
- If you have no STI symptoms, learn about whether a GYT screening may be a good option.
What's the difference between treatable and curable?
All STIs are treatable and many STIs are curable. STIs can either be caused by viruses, bacteria, or parasites. Bacterial and parasitic STIs are treated by antibiotics and other medications and thus often curable. Viral STIs such as HIV, HPV, Herpes, and Hepatitis—the four Hs—generally have no cure, but many symptoms can be alleviated with treatment.
What should I do if I am showing symptoms?
Make an appointment with a provider at the student health center or with a provider in the community as soon as possible. They will help you get tested for STIs and get treatment.
How should I inform my partners?
Be honest. There is nothing shameful about having an STI. Let them know the facts and encourage them to also get tested and seek treatment. Decide how much information you feel comfortable sharing and set boundaries. For more ideas on how to comfortably and safely disclose your status, check here or here. You can also let your partner(s) know completely anonymously that they should get tested by sending them a text message!
- “Hey I need to talk to you about something important... I’ve been diagnosed with ____ and I’m getting treated. It’s probably a good idea for you to also get tested to see if you need treatment as well”
Can I get an STI from oral sex?
You sure can. Although oral sex is often considered “safer” than vaginal or anal sex, you can get STIs from both giving or receiving oral sex. Many STIs including chlamydia, gonorrhea, and herpes can be transmitted through oral sex. It is a good idea to use barrier methods like condoms (internal or external) or dental dams in order to prevent fluid transfer and reduce your risk of catching an STI.
How do I ask my partner about their status?
If you can, try to have the conversation before things start heating up. One strategy is to sandwich the conversation between positive things you feel about the relationship.
- “I really like you and value you our relationship. I was thinking that before we take things to the next level it might be a good idea to talk about our sexual health and the last time we got tested? I definitely don’t want to kill the mood, but I find you really attractive and really want to take this to the next level.”
- Try to avoid asking your partner(s) if they are clean as this assigns stigma to having an STI.
- Since STIs often are asymptomatic, it’s possible that your partner(s) may not even know that they have an STI. The only way to be sure of your and their status is to get tested! Until you and your(s) get tested together, its best to operate under the assumption that they have an STI and practice the safest sex possible, including barrier methods.
Can I get an STI more than once?
After getting treatment, your body does not build immunity to any bacterial or parasitic STI so you can get a STI multiple times. You can prevent reinfection by completing your entire treatment, having your partner(s) get tested and treated, and practicing safer sex.
Sexual Empowerment
Sex Communication Checklist
Use this checklist to help you think through and evaluate your sexual wants, needs, and limits. You can even decide to share your answers with a partner or use some of the questions to guide conversations with each other.
Sex Ed Quickies: Sex Communication
Watch this video from the Well's Health Promotion team focused on talking about sex and communicating with partners.
The Clitoris
Learn more about the clitoris here. The clitoris is the only part of human anatomy whose sole function is to experience pleasure.

Bang: Masturbation Nation - A Sex-Ed Zine for all Genders and Genitalia
Check out this zine that was designed by Vic Liu for all genders and genitalia which goes in depth in masturbation.
Sex Ed Quickies: Masturbation
Watch this video by the Well's Health Promotion team talking about masturbation as sexual self-care.
Coming Soon
Learn about boundaries and how to protect yours from the Well for Health Promotion team: